The
ST segment is the flat, isoelectric section of the ECG between the end of the S wave (the J point) and the beginning of the T wave.
- The ST Segment represents the interval between ventricular depolarization and repolarization.
- The most important cause of ST segment abnormality (elevation or depression) is myocardial ischaemia or infarction.
Morphology of the Elevated ST segment
Myocardial Infarction
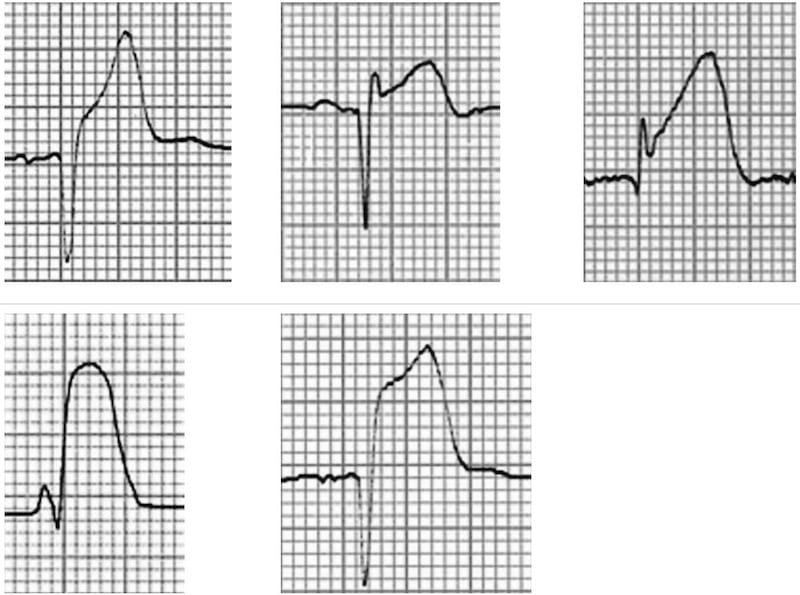
Acute STEMI may produce ST elevation with either concave, convex or obliquely straight morphology.
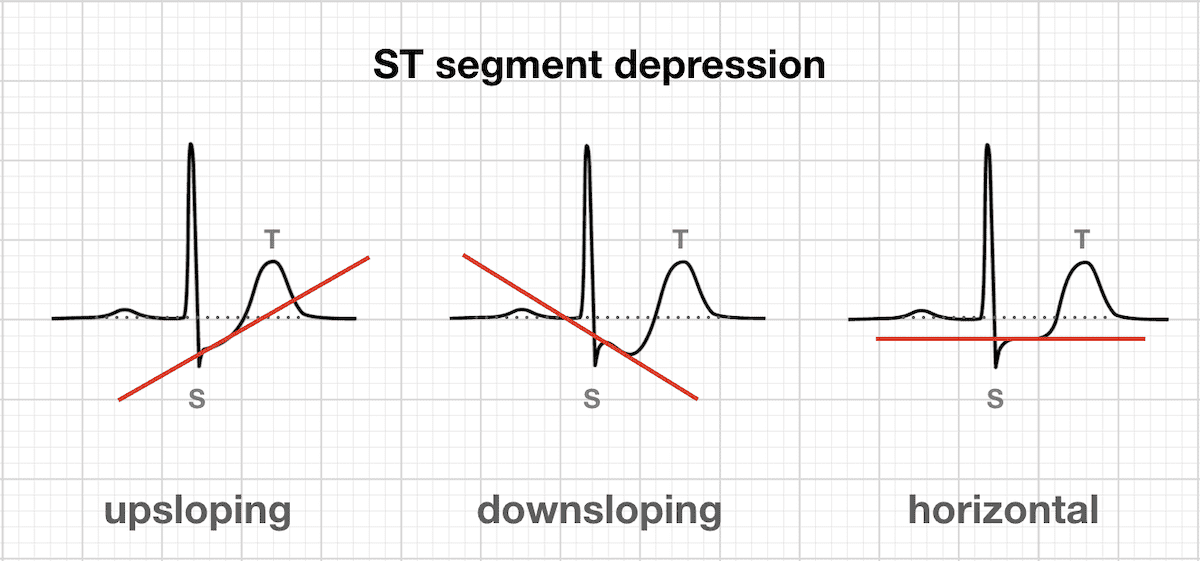
Morphology of ST Depression
- ST depression can be either upsloping, downsloping, or horizontal.
- Horizontal or downsloping ST depression ≥ 0.5 mm at the J-point in ≥ 2 contiguous leads indicates myocardial ischaemia.
- Upsloping ST depression in the precordial leads with prominent De Winter T waves is highly specific for occlusion of the LAD.
- Reciprocal change has a morphology that resembles “upside down” ST elevation and is seen in leads electrically opposite to the site of infarction.
- Posterior MI manifests as horizontal ST depression in V1-3 and is associated with upright T waves and tall R waves.
ST Segment depression
[SOURCE: LITFL - ST Segment]